For those who question whether masks work, here are several scientific experiments and studies that support the recommendation that we should all be wearing masks when out in public.
The first four articles in the list are videos. The next one is a good summary of mask issues. Next are short excerpts from a variety of scientific articles, The last is a list of additional scientific studies that I found at the end!
Live Science
Visualization shows exactly how face masks stop COVID-19 transmission
https://www.livescience.com/face-mask-visualization-droplets-covid-19.html
It’s Ok to be Smart: How Well Do Masks Work?
“Wearing a mask ‘s OK to be Smis a cheap and easy way to help stop the spread of airborne infections like COVID-19. It’s also a sign that you want to help protect other people and have them protect you… that we’re all in this together. Here are some awesome slow-motion schlieren imaging experiments to demonstrate why masks work!”
https://www.pbs.org/video/how-well-do-masks-work-ke2qje/
It’s Ok to be Smart: COVID-19 & Mask Myths DEBUNKED!
https://www.youtube.com/watch?v=npXP5wqNzaI
https://www.nbcphiladelphia.com/news/coronavirus/face-masks-greatly-reduce-risk-of-covid-19-watch-this-video-to-see-how/2435392/
University of California San Francisco
Still Confused About Masks? Here’s the Science Behind How Face Masks Prevent Coronavirus
By Nina Bai
https://www.ucsf.edu/news/2020/06/417906/still-confused-about-masks-heres-science-behind-how-face-masks-prevent
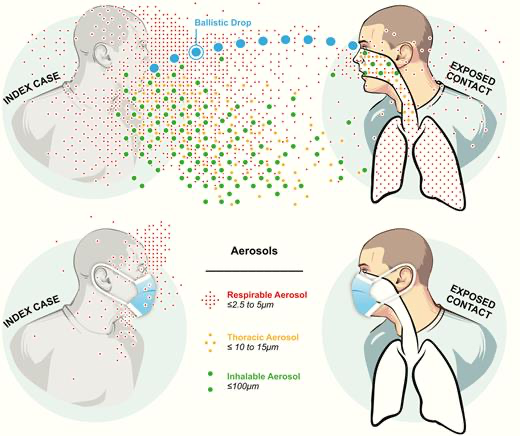
The Journal of the Pediatric Infectious Diseases
“A Rosetta Stone for Understanding Infectious Drops and Aerosols”
Proceedings of the National Academy of Sciences of the United States of America (PNAS)
Identifying airborne transmission as the dominant route for the spread of COVID-19
“We have elucidated the transmission pathways of coronavirus disease 2019 (COVID-19) by analyzing the trend and mitigation measures in the three epicenters. Our results show that the airborne transmission route is highly virulent and dominant for the spread of COVID-19. The mitigation measures are discernable from the trends of the pandemic. Our analysis reveals that the difference with and without mandated face covering represents the determinant in shaping the trends of the pandemic. This protective measure significantly reduces the number of infections. Other mitigation measures, such as social distancing implemented in the United States, are insufficient by themselves in protecting the public. Our work also highlights the necessity that sound science is essential in decision-making for the current and future public health pandemics.”
Proceedings of the Royal Society – The Royal Society Publishing
A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down’ in managing the COVID-19 pandemic
Preprints 2020
Face Masks Against COVID-19: An Evidence Review
Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.; Tang, V.; Watson, G.L.; Bax, C.E.; Shaikh, R.; Questier, F.; Hernandez, D.; Chu, L.F.; Ramirez, C.M.; Rimoin, A.W. Face Masks Against COVID-19: An Evidence Review. Preprints 2020, 2020040203 (doi: 10.20944/preprints202004.0203.v2).
“The science around the use of masks by the general public to impede COVID-19 transmission is advancing rapidly. Policymakers need guidance on how masks should be used by the general population to combat the COVID-19 pandemic. Here, we develop an analytical framework to examine an overlooked aspect of mask usage: masks as source-control targeting egress from the wearer with benefits at the population-level, rather than as PPE used for ingress control for health-care workers with focus on individual outcomes. We consider and synthesize the relevant literature to inform multiple areas: 1) transmission characteristics of COVID-19, 2) filtering characteristics and efficacy of masks, 3) estimated population impacts of widespread community mask use, and 4) sociological considerations for policies concerning mask-wearing. A primary route of transmission of COVID-19 is likely via respiratory droplets, and is known to be transmissible from presymptomatic and asymptomatic individuals. Reducing disease spread requires two things: first, limit contacts of infected individuals via physical distancing and other measures, and second, reduce the transmission probability per contact. The preponderance of evidence indicates that mask wearing reduces the transmissibility per contact by reducing transmission of infected droplets in both laboratory and clinical contexts. Public mask wearing is most effective at reducing spread of the virus when compliance is high. The decreased transmissibility could substantially reduce the death toll and economic impact while the cost of the intervention is low. Given the current shortages of medical masks we recommend the adoption of public cloth mask wearing, as an effective form of source control for now, in conjunction with existing hygiene, distancing, and contact tracing strategies. We recommend that public officials and governments strongly encourage the use of widespread face masks in public, including the use of appropriate regulation.”
The Lancet
Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis
Derek K Chu, MD; Prof Elie A Akl, MD; Stephanie Duda, MSc; Karla Solo, MSc; Sally Yaacoub, MPH; Prof Holger J Schünemann, MD, et al. Open AccessPublished:June 01, 2020DOI:https://doi.org/10.1016/S0140-6736(20)31142-9
“The findings of this systematic review and meta-analysis support physical distancing of 1 m or more and provide quantitative estimates for models and contact tracing to inform policy. Optimum use of face masks, respirators, and eye protection in public and health-care settings should be informed by these findings and contextual factors.”
Heath Affairs
Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US
Wei Lyu and George L. Wehby PUBLISHED:JUNE 16, 2020 Free Access https://doi.org/10.1377/hlthaff.2020.00818
“State policies mandating public or community use of face masks or covers in mitigating novel coronavirus disease (COVID-19) spread are hotly contested. This study provides evidence from a natural experiment on effects of state government mandates in the US for face mask use in public issued by 15 states plus DC between April 8 and May 15. The research design is an event study examining changes in the daily county-level COVID-19 growth rates between March 31, 2020 and May 22, 2020. Mandating face mask use in public is associated with a decline in the daily COVID-19 growth rate by 0.9, 1.1, 1.4, 1.7, and 2.0 percentage-points in 1–5, 6–10, 11–15, 16–20, and 21+ days after signing, respectively. Estimates suggest as many as 230,000–450,000 COVID-19 cases possibly averted By May 22, 2020 by these mandates. The findings suggest that requiring face mask use in public might help in mitigating COVID-19 spread.”
Research Gate
Association of country-wide coronavirus mortality with demographics, testing, lockdowns, and public wearing of masks (Update June 15, 2020).
Leffler, Christopher & Ing, Edsel & Lykins, Joseph & Hogan, Matthew & McKeown, Craig & Grzybowski, Andrzej. (2020). Association of country-wide coronavirus mortality with demographics, testing, lockdowns, and public wearing of masks (Update June 15, 2020)..
“Conclusions. Societal norms and government policies supporting the wearing of masks by the public, as well as international travel controls, are independently associated with lower per-capita mortality from COVID-19.”
Centers for Disease Control and Prevention
Effectiveness of Cloth Masks for Protection Against Severe Acute Respiratory Syndrome Coronavirus 2
Chughtai AA, Seale H, Macintyre CR. Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis 2020 Oct [date cited]. DOI: 10.3201/eid2610.200948. Original Publication Date: July 22, 2020
“Cloth masks have been used in healthcare and community settings to protect the wearer from respiratory infections. The use of cloth masks during the coronavirus disease (COVID-19) pandemic is under debate. The filtration effectiveness of cloth masks is generally lower than that of medical masks and respirators; however, cloth masks may provide some protection if well designed and used correctly. Multilayer cloth masks, designed to fit around the face and made of water-resistant fabric with a high number of threads and finer weave, may provide reasonable protection. Until a cloth mask design is proven to be equally effective as a medical or N95 mask, wearing cloth masks should not be mandated for healthcare workers. In community settings, however, cloth masks may be used to prevent community spread of infections by sick or asymptomatically infected persons, and the public should be educated about their correct use.”
NHPR interview
Growing Body Of Evidence Suggests Masks Protect Those Wearing Them, Too
And, now that I’ve gone this far, I found this list of “Recent Studies” from the CDC.
(Confession: I haven’t investigated these!)
- Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. The New England journal of medicine. 2020;382(10):970-971. PMID: 32003551external icon
- Zou L, Ruan F, Huang M, et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. The New England journal of medicine. 2020;382(12):1177-1179. PMID: 32074444external icon
- Pan X, Chen D, Xia Y, et al. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. The Lancet Infectious diseases. 2020. PMID: 32087116external icon
- Bai Y, Yao L, Wei T, et al. Presumed Asymptomatic Carrier Transmission of COVID-19. Jama. 2020. PMID: 32083643external icon
- Kimball A HK, Arons M, et al. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility — King County, Washington, March 2020. MMWR Morbidity and mortality weekly report. 2020; ePub: 27 March 2020. PMID: 32240128external icon
- Wei WE LZ, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;ePub: 1 April 2020. PMID: 32271722external icon
- Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science (New York, NY). 2020. PMID: 32179701external icon
- Furukawa NW, Brooks JT, Sobel J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic [published online ahead of print, 2020 May 4]. Emerg Infect Dis. 2020;26(7):10.3201/eid2607.201595. Link
- Oran DP, Topol Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review [published online ahead of print, 2020 Jun 3]. Ann Intern Med. 2020;M20-3012. PMID: 32491919external icon
- National Academies of Sciences, Engineering, and Medicine. 2020. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (April 1, 2020). Washington, DC: The National Academies Press. https://doi.org/10.17226/25769external icon.
- Schwartz KL, Murti M, Finkelstein M, et al. Lack of COVID-19 transmission on an international flight. CMAJ. 2020;192(15):E410. PMID: 32392504external icon
- Anfinrud P, Stadnytskyi V, Bax CE, Bax A. Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering. N Engl J Med. 2020 Apr 15. doi:10.1056/NEJMc2007800. PMID: 32294341external icon
- Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013;7(4):413-8. PMID: 24229526external icon
- Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano. 2020 Apr 24. PMID: 32329337external icon
- Aydin O, Emon B, Saif MTA. Performance of fabrics for home-made masks against spread of respiratory infection through droplets: a quantitative mechanistic study. medRxiv preprint doi: https://doi.org/10.1101/2020.04.19.20071779, posted April 24, 2020.
- Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020. PMID: 32232986external icon
- Leung, N.H.L., Chu, D.K.W., Shiu, E.Y.C. et al.Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020. PMID: 32371934external icon
- Johnson DF, Druce JD, Birch C, Grayson ML. A quantitative assessment of the efficacy of surgical and N95 masks to filter influenza virus in patients with acute influenza infection. Clin Infect Dis. 2009 Jul 15;49(2):275-7. PMID: 19522650external icon
- Green CF, Davidson CS, Panlilio AL, et al. Effectiveness of selected surgical masks in arresting vegetative cells and endospores when worn by simulated contagious patients. Infect Control Hosp Epidemiol. 2012;33(5):487‐494. PMID: 22476275external icon

